One in two Americans will develop a musculoskeletal condition in their lifetime. Injuries, overuse or underuse, and even stress can all contribute to symptoms. Treatment approaches should be tailored to individual pain experiences, but often, musculoskeletal pain is treated with a “one size fits all” care program.
Personalized musculoskeletal employer programs – like Fern – have the potential to improve outcomes by directing people in pain away from ineffective, costly and potentially harmful treatments to safe and more effective programs.
How can musculoskeletal pain management be personalized?
In some cases, the cause of pain and the solution are relatively clear-cut. Someone might have an acute injury to their back and feel better in a few weeks with exercise and active recovery, while for others, their pain sticks around.
When pain lasts for 12 weeks or longer, it’s considered persistent – and becomes more complex. The brain and spinal cord produce the experience of pain, and input from other body tissue such as nerves, muscles, and joints can also contribute. In many cases, persistent pain is non-specific, in that no one specific injury or tissue is contributing to the pain experience. Often, psychological and social aspects impact recovery from persistent pain.
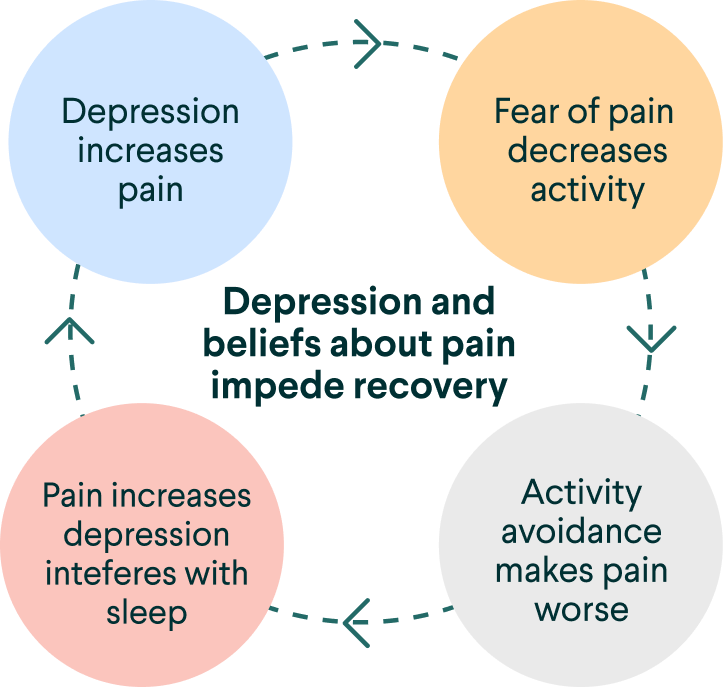
While exercise and physical activity are key to modify the experience of pain, psychological and social factors such as fear, anxiety, and depression can make it difficult to start.
For example, someone with a fear of movement, or kinesiophobia, may not be able to even begin an exercise therapy program or make much progress if the psychological side of their pain isn’t addressed. In this way, adjusting peoples’ programs to match social and psychological challenges is critical to achieve meaningful improvement in symptoms.
How Fern Health is advancing personalization in musculoskeletal employer programs
We can identify groups of people with different symptoms, medical history, demographics and lifestyles that are more likely to respond to one treatment over another – but you need a large amount of data to draw accurate conclusions. Through our collaboration with Massachusetts General Hospital, we’ll incorporate 10 million de-identified health records into the Fern platform to create personalized pain care paths.
When new members join Fern, we’ll identify personalized care pathways that have worked for people with backgrounds and pain experiences like theirs. Data from the Fern program is also used to personalize their plan by changing in response to input from the member as they move through it.
Because Fern is built on a foundation of pain neuroscience education, exercise therapy, and health coaching, the program modulations include both exercise adjustments and suggestions based on neuroscience principles. For example, a member who experiences pain catastrophizing may receive additional interactive modules designed to help them rewire their pain reactions and find relief.
Overall, pain treatment in the U.S. is not targeted enough. Physicians order MRI scans or even recommend surgery before patients have the opportunity to try physical therapy. Only 8% of people with chronic back pain receive cognitive behavioral therapy, despite guidelines recommending otherwise.
Self-insured employers reduce MSK pain costs and improve outcomes for employees with back pain and other joint pain by offering digital, personalized care. Corporate chronic MSK programs like Fern democratize who can access the highest-quality, most effective care, while creating pathways that work best for each individual pain experience. Fern can also identify and treat the underlying contributors to pain, such as anxiety and depression, in ways that traditional approaches can’t.
Want to learn more about Fern Health’s customized chronic pain program? Get in touch using the form below.






